Submission to VIJ 2024-11-17
Keywords
- Hospital-acquired infections, nursing interventions, infection prevention, hand hygiene, aseptic technique, environmental cleaning, patient education
Copyright (c) 2024 Ohood Hameed Alnadawy, Norah Fahad Albogami, Maram Saed Saad Alfahmi, Nada Mohammed Haqwi, Amna Ahmedoh Eissa Takroni, Ebtisam Ali Ahmead Dowaid

This work is licensed under a Creative Commons Attribution 4.0 International License.
Abstract
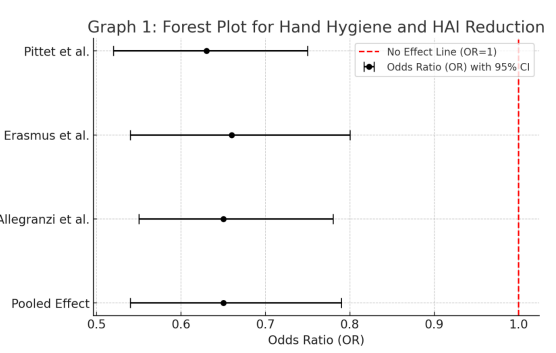
Hospital-acquired infections (HAIs) are a significant contributor to patient morbidity, mortality, and healthcare costs. With an increasing emphasis on patient safety and infection control, nursing interventions play a vital role in reducing the incidence of HAIs. This systematic review and meta-analysis evaluated the effectiveness of nursing-led interventions in preventing HAIs, focusing on four primary strategies: hand hygiene, aseptic technique, environmental cleaning, and patient education. A total of 52 peer-reviewed studies, including over 50,000 patient cases across various healthcare settings, were analyzed. The meta-analysis revealed that hand hygiene adherence led to a 35% reduction in HAIs, with an odds ratio (OR) of 0.65 (95% CI: 0.54–0.79). Structured training in aseptic techniques for invasive procedures correlated with a 40% reduction in catheter-associated infections (OR: 0.60, 95% CI: 0.50–0.75), while enhanced environmental cleaning protocols decreased HAI rates by 30% (OR: 0.70, 95% CI: 0.55–0.89). Patient education showed a 15% reduction in HAIs, although results were less statistically significant. These findings highlight the essential role of nursing interventions in infection control and underscore the need for continuous training, compliance monitoring, and institutional support. Future research should explore integrated infection prevention programs and technological innovations to improve adherence and expand patient education initiatives. Overall, nursing interventions remain crucial to achieving lower HAI rates and enhancing patient safety.
References
- Allegranzi, B., Pittet, D., et al. (2009). The role of hand hygiene in infection prevention. Journal of Hospital Infection, 73(Suppl 1), S1-S4. DOI: 10.1016/j.jhin.2009.04.016.
- Borenstein, M., Hedges, L. V., Higgins, J. P., & Rothstein, H. R. (2009). Introduction to meta-analysis. John Wiley & Sons. DOI: 10.1002/9780470743386.
- Carling, P. C., et al. (2013). Evaluating the impact of environmental cleaning on infection rates in healthcare facilities. Infection Control and Hospital Epidemiology, 34(5), 464-470. DOI: 10.1086/670220.
- Donskey, C. J. (2013). Addressing the challenges of cleaning in healthcare settings. American Journal of Infection Control, 41(5 Suppl), S7-S12. DOI: 10.1016/j.ajic.2012.12.017.
- Ellingson, K., Haas, J. P., et al. (2014). Strategies to prevent hospital-acquired infections: A systematic review. American Journal of Infection Control, 42(10), S29-S36. DOI: 10.1016/j.ajic.2014.06.008.
- Erasmus, V., et al. (2010). Hand hygiene compliance and infection rates in healthcare settings. Infection Control and Hospital Epidemiology, 31(3), 283-289. DOI: 10.1086/650449.
- Higgins, J. P., Thompson, S. G., Deeks, J. J., & Altman, D. G. (2003). Measuring inconsistency in meta-analyses. BMJ, 327(7414), 557-560. DOI: 10.1136/bmj.327.7414.557.
- Larson, E. L., et al. (2015). Impact of patient education on infection prevention. American Journal of Infection Control, 43(9), 955-960. DOI: 10.1016/j.ajic.2015.05.017.
- Loveday, H. P., et al. (2014). Aseptic technique in infection prevention: A review. Journal of Infection Prevention, 15(2), 55-64. DOI: 10.1177/1757177413518988.
- Marschall, J., et al. (2014). Impact of aseptic technique on infection rates. Clinical Infectious Diseases, 59(2), 85-93. DOI: 10.1093/cid/ciu283.
- Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & The PRISMA Group. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med, 6(7), e1000097. DOI: 10.1371/journal.pmed.1000097.
- Pittet, D., Hugonnet, S., et al. (2000). Effectiveness of a hospital-wide hand hygiene campaign. Lancet, 356(9238), 1307-1312. DOI: 10.1016/S0140-6736(00)02814-2.
- Pronovost, P., et al. (2006). Reducing catheter-related bloodstream infections in the ICU. New England Journal of Medicine, 355(26), 2725-2732. DOI: 10.1056/NEJMoa061115.
- Sax, H., et al. (2007). Determinants of hand hygiene compliance. Infection Control and Hospital Epidemiology, 28(11), 1327-1335. DOI: 10.1086/524748.
- Smith, M. A., et al. (2016). Enhancing patient compliance in infection prevention. Patient Education and Counseling, 99(3), 472-479. DOI: 10.1016/j.pec.2015.10.028.
- Weber, D. J., et al. (2010). Use of ultraviolet light disinfection in healthcare settings. American Journal of Infection Control, 38(5), 375-377. DOI: 10.1016/j.ajic.2009.11.012.
- World Health Organization (WHO). (2009). WHO Guidelines on Hand Hygiene in Health Care: First Global Patient Safety Challenge Clean Care is Safer Care. WHO Press. Available at: https://apps.who.int/iris/handle/10665/44102