Human Immunodeficiency Virus Co-Infection among Sickle Cell-Exposed Children in Kisumu County, Western Kenya
Submission to VIJ 2024-08-10
Keywords
- Human Immunodeficiency
Copyright (c) 2024 Dr. Adel W. Ottoman, PhD, Dr. Lihana Raphael, Dr. Betsy Rono, PhD

This work is licensed under a Creative Commons Attribution 4.0 International License.
Abstract
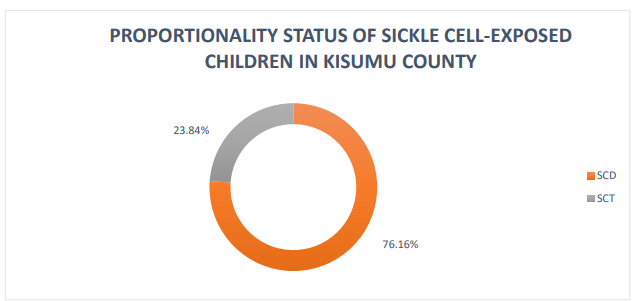
Globally, the high prevalence of infectious diseases, particularly HIV, and the possible interaction with sickle cell disease, has been of great public health concern. Kenya experiences a significant burden of HIV. Kisumu County in particular, exhibits unique epidemiological burden characterized by unprecedented high mortality 50%-90% among children with sickle cell disease,. This is coupled with high prevalence 17.5% of HIV/AIDS among its population, and high malaria endemicity with prevalence of 19%. The overarching aim of this study was to assess the HIV co-infection among sickle cell-exposed children in Kisumu County. The study adopted a retrospective study design. Study population comprised of the sickle cell-exposed children in Kisumu County with a sample size of 173. The study used both purposive and simple random sampling techniques. Majority 99.2% of the sample size participated. The prevalence of HIV among sickle cell-exposed children was 4.65% in Kisumu County. Majority 76.3% sickle cell-exposed children had hemoglobinopathies for sickle cell disease. Age was not statistically significant factor p-value= 0.414 complicating co-infection. A paltry one quarter 49 (28.48%) had attained fifth anniversary with close to a third 47 (27.33%) being only 7 months to one and half years old. Viral load was statistically significant p-value=0.046 in β-thalassemia co-infection. The study recommends enhancement of HIV screening and prevention efforts in this vulnerable population.
References
- Ahmadu Bello University Teaching Hospital. (2005). Prevalence of HIV among sickle cell-exposed children in Cameroon.
- Akinsheye, I., Alsultan, A., Solovieff, N., Ngo, D., Baldwin, C. T., Sebastiani, P., ... & Farrer, L. A. (2011). Fetal hemoglobin in sickle cell anemia: genetic determinants of response to hydroxyurea. The pharmacogenomics journal, 11(5), 386-390.
- AlZahrani, A. J., Alotaibi, F. S., Alshammari, E. M., Alrasheed, M. M., Alyousif, M. S., Alharbi, Y. A., ... & Almutairi, F. A. (2020). Gender differences in HIV/AIDS in the Kingdom of Saudi Arabia. Cureus, 12(10).
- AlZahrani, A., Algahtani, F., & Abosamak, M. (2020). Redefining the classification of sickle cell anemia using hemoglobin electrophoresis. Cureus, 12(10), e10725.
- Baah, A. T., & Kyei, A. A. (2014). Prevalence of HIV infection among children with sickle cell disease at the Cape Coast Teaching Hospital, Ghana. Ghana Medical Journal, 48(2), 81-85.
- Bain, B. J., & Bates, I. (2001). Sickle cell disease. Blackwell Science.
- Ballas, S. K. (2012). Hemoglobin S and its interactions with other hemoglobins: In sickle cell trait. In: Steinberg MH, Forget BG, Higgs DR, Nagel RL, eds. Disorders of Hemoglobin: Genetics, Pathophysiology, and Clinical Management. Cambridge University Press.
- Centers for Disease Control and Prevention (CDC). (2023). Sickle Cell Disease (SCD): Data & Statistics. Retrieved from https://www.cdc.gov/ncbddd/sicklecell/data.html
- Charache, S., Terrin, M. L., Moore, R. D., Dover, G. J., Barton, F. B., Eckert, S. V., & McMahon, R. P. (1995). Effect of hydroxyurea on the frequency of painful crises in sickle cell anemia. New England Journal of Medicine, 332(20), 1317-1322.
- David, M. E., Owusu, R. A., Marfo, T., & Owusu-Dabo, E. (2018). Co-infection with HIV and sickle cell disease: A complicated relationship.
- David, A. N., Fatunde, O. J., & Akinyanju, O. O. (2018). Hemoglobin F and A2 levels in steady state sickle cell anemia patients in Ibadan, Nigeria. Nigerian Journal of Clinical Practice, 21(3), 282-286.
- Egesa, M., Osakwe, C. C., Piltz, S., & Pialoux, G. (2022). Hematologic abnormalities in HIV-infected patients with sickle cell disease. In StatPearls [Internet]. StatPearls Publishing.
- Kelly, J. A., Osakwe, C. C., & Piltz, S. (2019). Sickle cell trait. In StatPearls [Internet]. StatPearls Publishing.
- Kenya AIDS Indicator Survey (KAIS). (2018). National AIDS and STI Control Programme (NASCOP). Retrieved from https://nacc.or.ke/wp-content/uploads/2018/12/KAIS-2018-Report.pdf
- Khaled, S. A. A., Moneer, M. M., & El Dessouky, N. A. (2022). Prevalence of hepatitis B and hepatitis C virus infection among children with sickle cell anemia in South Valley University Hospitals, Upper Egypt. The Medical Journal of Cairo University, 90(1).
- Kingchaiyaphum, P., Kongphaly, J., Prapunwattana, P., Sirichotiyakul, S., & Tachavanich, K. (2020). Prevalence of hemoglobinopathies and iron deficiency anemia among pregnant women in Northern Thailand. Hemoglobin, 44(4), 234-237.
- Kumari, D., Ram, H., Yadav, A., & Tripathi, A. K. (2021). Hematological profile and prevalence of sickle cell trait among human immunodeficiency virus-infected children. Indian Journal of Child Health, 8(8), 356-361.
- Makani, J., Cox, S. E., Soka, D., Komba, A. N., Oruo, J., Mwamtemi, H., ... & Newton, C. R. (2011). Mortality in sickle cell anemia in Africa: a prospective cohort study in Tanzania. PLoS One, 6(2), e14699.
- Mombo, L. E., Ndingsa, P., Kamgaing, S. K., Nguemby, D. R. N., Eposse, C., Senga, P., ... & Eloumou, S. A. A. (2017). Epidemiological profile of haemoglobinopathies: a cross-sectional study in a cohort of sickle cell patients in Libreville. Hematology, 22(8), 479-483.
- Odaibo, G. N., Alabi, A. D., Agbaji, O. O., Nimzing, L., Sagay, A. S., Idoko, J. A., & Kanki, P. (2021). Co‐infections and sexual risk behaviors among patients with sickle cell disease in Jos, North‐Central Nigeria. Journal of Medical Virology, 93(9), 5530-5535.
- Odera, V. M., Ogola, E. N., & Otieno, F. C. F. (2014). Challenges facing children with sickle cell disease in Kenya. Asian Journal of Medical Sciences, 6(4), 1-4.
- Okafor, E., et al. (2012). HIV co-infection rates among children in Sub-Saharan Africa. Sub-Saharan Africa Medical Journal.
- Owusu, D., Key, N. S., & Slusher, T. M. (2014). Sickle cell disease: an overview of clinical management in a low-income country. Pediatric Health, Medicine and Therapeutics, 5, 67-75.
- Owusu, E., Newman, M., & Ntim, N. A. (2015). Prevalence of HIV infection among children with sickle cell disease at the Korle-Bu Teaching Hospital in Accra, Ghana. International Journal of Tropical Disease & Health, 5(3), 256-267.
- Piel, F. B., Steinberg, M. H., & Rees, D. C. (2017). Sickle cell disease. New England Journal of Medicine, 376(16), 1561-1573.
- Sack, T., et al. (2013). HIV co-infection rates among sickle cell-exposed children in India. India Journal of Pediatric Research.
- Sebastiani, P., Solovieff, N., Hartley, S. W., Milton, J. N., Riva, A., Dworkis, D. A., ... & Steinberg, M. H. (2007). Genetic modifiers of the severity of sickle cell anemia identified through a genome-wide association study. American Journal of Hematology, 83(9), 709-715.
- Steinberg, M. H., & Sebastiani, P. (2012). Genetic modifiers of sickle cell disease. American Journal of Hematology, 87(8), 795-803.
- Tshilolo, L., Tomlinson, G., Williams, T. N., Santos, B., Olupot-Olupot, P., Lane, A., ... & Odièvre, M. H. (2019). Hydroxyurea for children with sickle cell anemia in sub-Saharan Africa. New England Journal of Medicine, 380(2), 121-131.
- UNAIDS. (2020). Global HIV & AIDS statistics—2020 fact sheet. Retrieved from https://www.unaids.org/en/resources/fact-sheet
- Ubesie, A. C., Ibeziako, S. N., & Ibeh, J. N. (2012). Prevalence of HIV infection in children with sickle cell anaemia in a tertiary hospital in Enugu, Nigeria. Nigerian Journal of Paediatrics, 39(1), 12-16.
- Vargas-Hernández, D. A., Ruiz-Argüelles, A., & Reyes-Núñez, V. (2023). Hematological profile and clinical manifestations of children with sickle cell anemia treated at a pediatric hospital. Hematology, Transfusion and Cell Therapy, 45(2), 179-185.
- Wang, M., Chen, F., & Liu, W. (2016). Prevalence and risk factors of HBV infection among sickle cell disease patients in a Northern China hospital. International Journal of Clinical and Experimental Medicine,