Sickle Cell Disease Pain and Zinc, Any Link? A Case-Control Study among Patients With Sickle Cell Disease In Korle-Bu
Submission to VIJ 2024-08-01
Keywords
- zinc,
- trace element,
- sickle cell disease,
- pain,
- atomic absorption spectroscopy
Copyright (c) 2024 Dr. GK Ababio , Dr. Ababio Boateng, Dr. EV Asare, Mr. R Reeks, Dr. Dongdem

This work is licensed under a Creative Commons Attribution 4.0 International License.
Abstract
Background: Over some few decades, markers of pain have been studied, of which some trace elements are of no exception. Yet, there is paucity of data on trace elements in SCD pain. Here, zinc levels and its relation to SCD vaso-occlusive pain was shown.
Aim: To determine [zinc] and its relation to pain in sickle cell disease patients.
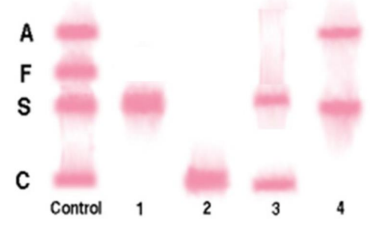
Methodology: The case-control study was located at the Ghana Institute of Clinical Genetics (sickle cell clinic). After obtaining ethical clearance from College of Health Sciences (CHS-Et/M.1-P5.12/2023-2024), a validated pain assessment questionnaires were used for data collection. Ten (10) mls of blood was collected, six (6) mL was placed in a serum separating tube (SST) for the determination of zinc and four (4) mL into EDTA tube for full blood count and Hemoglobinopathy on cellulose acetate electrophoresis. The data analysis was done using the Statistical Package for the Social Science (SPSS) version 21 and Microsoft Excel 2016.
Results: Average zinc levels for the entire SCD VOC, was 2.569±1.073(39) and this was relatively low during comparison. [Zn] in SCD subjects who consume alcohol yielded p – value of 0.0001 while in patients experiencing VOC had a p-value = 0.000. The odds ratio for zinc exposure seemed to have protective effect on sickle cell disease either in steady state or vaso-occlusive state. [Zn] stratifications also related statistically to blood pressure readings, SCD pain, hemoglobin, red blood cells, white blood cells, platelets and body mass index. Conclusion: The average [Zn] in SCD individuals experiencing VOC was relatively low (p-value = 0.000
References
- Ballas SK, Darbari DS. Review/overview of pain in sickle cell disease. Complementary Therapies in Medicine. 2020;49:102327.
- Saraf SL, Molokie RE, Nouraie M, Sable CA, Luchtman-Jones L, Ensing GJ, Campbell AD, Rana SR, Niu XM, Machado RF, Gladwin MT. Differences in the clinical and genotypic presentation of sickle cell disease around the world. Paediatric respiratory reviews. 2014;15(1):4-12.
- Asare EV, Wilson I, Benneh-Akwasi Kuma AA, Dei-Adomakoh Y, Sey F, Olayemi E. Burden of sickle cell disease in Ghana: The Korle‐Bu experience. Advances in hematology. 2018;2018(1):6161270.
- Ampomah MA, Drake JA, Anum A, Amponsah B, Dei‐Adomakoh Y, Anie K, Mate‐Kole CC, Jonassaint CR, Kirkham FJ. A case‐control and seven‐year longitudinal neurocognitive study of adults with sickle cell disease in Ghana. British Journal of Haematology. 2022;199(3):411-26.
- de Oliveira Fernandes Miranda CT, Vermeulen-Serpa KM, Cabanas Pedro AC, Brandao-Neto J, de Lima Vale SH, Figueiredo MS. Zinc in sickle cell disease: A narrative review. Journal Of Trace Elements In Medicine And Biology. 2022;72:126980
- Swe KM, Abas AB, Bhardwaj A, Barua A, Nair NS. Zinc supplements for treating thalassaemia and sickle cell disease. Cochrane Database of Systematic Reviews. 2013(6).
- Prasad AS. Impact of the discovery of human zinc deficiency on health. Journal of trace elements in medicine and biology. 2014;28(4):357-63.
- Prasad AS. Discovery of zinc for human health and biomarkers of zinc deficiency. In Molecular, genetic, and nutritional aspects of major and trace minerals. 2017 (pp. 241-260). Academic Press.
- Temiye EO, Duke ES, Owolabi MA, Renner JK. Relationship between painful crisis and serum zinc level in children with sickle cell anaemia. Anemia. 2011;2011(1):698586.
- Abrams SA. Zinc deficiency and supplementation in children. Motil KJ, editor. 2020. https://medilib.ir/uptodate/show/5354
- Sharaf BK, Atrushi AM. Role of sickling crisis with serum zinc in children with sickle cell anemia. AMJ (Advanced Medical Journal). 2022;6(2):51-9.
- Namazzi R, Opoka R, Conroy AL, Datta D, Tagoola A, Bond C, Goings MJ, Ryu MS, Cusick SE, Krebs NF, Jang JH. Zinc for infection prevention in children with sickle cell anemia: a randomized double-blind placebo-controlled trial. Blood Advances. 2023 ;7(13):3023-31.
- Ugwu NI, Okike C, Ugwu CN, Ezeonu CT, Iyare FE, Alo C. Assessment of zinc level and its relationship with some hematological parameters among patients with sickle cell anemia in Abakaliki, Nigeria. Nigerian Journal of Medicine. 2021;30(1):55-9.
- Liu E, Pimpin L, Shulkin M, Kranz S, Duggan CP, Mozaffarian D, Fawzi WW. Effect of zinc supplementation on growth outcomes in children under 5 years of age. Nutrients. 2018;10(3):377.
- Ballas SK. More definitions in sickle cell disease: steady state v base line data. American journal of hematology. 2012;87(3):338.
- Nozaki C, Vergnano AM, Filliol D, Ouagazzal AM, Le Goff A, Carvalho S, Reiss D, Gaveriaux-Ruff C, Neyton J, Paoletti P, Kieffer BL. Zinc alleviates pain through high-affinity binding to the NMDA receptor NR2A subunit. Nature neuroscience. 2011;14(8):1017-22.
- Lima CK, Sisnande T, Silva RV, Silva VD, Amaral JJ, Ochs SM, Santos BL, Miranda AL, Lima LM. Zinc deficiency disrupts pain signaling promoting nociceptive but not inflammatory pain in mice. Anais da Academia Brasileira de Ciências. 2023;95(suppl 1):e20220914.
- Darbari DS, Ballas SK, Clauw DJ. Thinking beyond sickling to better understand pain in sickle cell disease. European journal of haematology. 2014;93(2):89-95.
- Tuerk MJ, Fazel N. Zinc deficiency. Current opinion in gastroenterology. 2009;25(2):136-43.
- Kloubert V, Wessels I, Wolf J, Blaabjerg K, Janssens V, Hapala J, Wagner W, Rink L. Zinc deficiency leads to reduced interleukin-2 production by active gene silencing due to enhanced CREMα expression in T cells. Clinical nutrition. 2021;40(5):3263-78.
- Yokokawa H, Fukuda H, Saita M, Miyagami T, Takahashi Y, Hisaoka T, Naito T. Serum zinc concentrations and characteristics of zinc deficiency/marginal deficiency among Japanese subjects. Journal of General and Family Medicine. 2020;21(6):248-55
- Nader E, Romana M, Connes P. The red blood cell—inflammation vicious circle in sickle cell disease. Frontiers in immunology. 2020;11:454.
- Gladwin MT, Kanias T, Kim-Shapiro DB. Hemolysis and cell-free hemoglobin drive an intrinsic mechanism for human disease. The Journal of clinical investigation. 2012;122(4):1205-8.
- Alayash AI. Hemoglobin-based blood substitutes and the treatment of sickle cell disease: more harm than help? Biomolecules. 2017;7(1):2.
- Ansari J, Gavins FN. Ischemia-reperfusion injury in sickle cell disease: from basics to therapeutics. The American Journal of Pathology. 2019;189(4):706-18.
- Zhang D, Xu C, Manwani D, Frenette PS. Neutrophils, platelets, and inflammatory pathways at the nexus of sickle cell disease pathophysiology. Blood, The Journal of the American Society of Hematology. 2016;127(7):801-9.
- Falih Neamah N, Naaeem Khudair AR, Al-Jadaan SA. In Vitro and in Vivo Measurements of ROS Scavenging Activity and White Blood Cells Activity by Chemiluminescence of a New Selena-Diazole Derivative Compare to Dipyrone Activity. In Journal of Physics Conference Series 2021;1818(1):012060.
- Bandeira IC, Rocha LB, Barbosa MC, Elias DB, Querioz JA, Freitas MV, Gonçalves RP. Chronic inflammatory state in sickle cell anemia patients is associated with HBB* S haplotype. Cytokine. 2014;65(2):217-21.
- Biswal S, Rizwan H, Pal S, Sabnam S, Parida P, Pal A. Oxidative stress, antioxidant capacity, biomolecule damage, and inflammation symptoms of sickle cell disease in children. Hematology. 2019;24(1):1-9.
- Xu Y, Li A, Li X, Deng X, Gao XJ. Zinc deficiency induces inflammation and apoptosis via oxidative stress in the kidneys of mice. Biological Trace Element Research. 2023;201(2):739-50.
- Prasad AS, Bao B. Molecular mechanisms of zinc as a pro-antioxidant mediator: clinical therapeutic implications. Antioxidants. 2019;8(6):164.
- Del Favero G, Hohenbichler J, Mayer RM, Rychlik M, Marko D. Mycotoxin altertoxin II induces lipid peroxidation connecting mitochondrial stress response to NF-κB inhibition in THP-1 macrophages. Chemical Research in Toxicology. 2020;33(2):492-504.
- Marreiro DD, Cruz KJ, Morais JB, Beserra JB, Severo JS, De Oliveira AR. Zinc and oxidative stress: current mechanisms. Antioxidants. 2017;6(2):24.
- Overbeck S, Rink L, Haase H. Modulating the immune response by oral zinc supplementation: a single approach for multiple diseases. Archivum immunologiae et therapiae experimentalis. 2008;56:15-30.
- Moheeb H, Wali YA, El‐Sayed MS. Physical fitness indices and anthropometrics profiles in schoolchildren with sickle cell trait/disease. American journal of hematology. 2007;82(2):91-7.
