Submission to VIJ 2024-01-18
Keywords
- hypertension, prevalence, metabolic syndrome, risk factors
Copyright (c) 2024 Ramez Ahmad Aqeel Matar, Aseel Fahed Faleh Aldamen, Esraa Mohammad Aqeel ‘Eial awwad’, Sara Mohammad Hussein Otoum, Dua’a Suleiman Hussein Alkhawaldeh

This work is licensed under a Creative Commons Attribution 4.0 International License.
Abstract
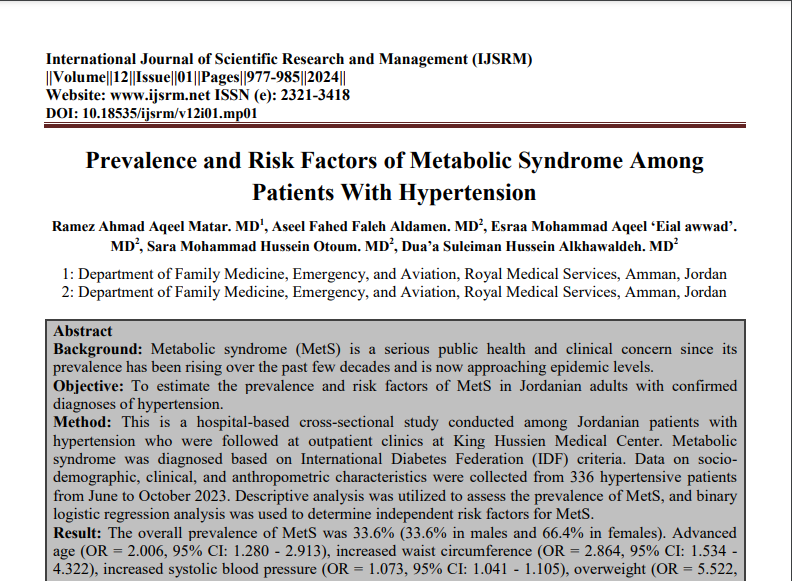
Background: Metabolic syndrome (MetS) is a serious public health and clinical concern since its prevalence has been rising over the past few decades and is now approaching epidemic levels.
Objective: To estimate the prevalence and risk factors of MetS in Jordanian adults with confirmed diagnoses of hypertension.
Method: This is a hospital-based cross-sectional study conducted among Jordanian patients with hypertension who were followed at outpatient clinics at King Hussien Medical Center. Metabolic syndrome was diagnosed based on International Diabetes Federation (IDF) criteria. Data on socio-demographic, clinical, and anthropometric characteristics were collected from 336 hypertensive patients from June to October 2023. Descriptive analysis was utilized to assess the prevalence of MetS, and binary logistic regression analysis was used to determine independent risk factors for MetS.
Result: The overall prevalence of MetS was 33.6% (33.6% in males and 66.4% in females). Advanced age (OR = 2.006, 95% CI: 1.280 - 2.913), increased waist circumference (OR = 2.864, 95% CI: 1.534 - 4.322), increased systolic blood pressure (OR = 1.073, 95% CI: 1.041 - 1.105), overweight (OR = 5.522, 95% CI: 1.371 - 7.422), and obesity (OR = 7.521, 95% CI: 4.520 - 9.016) were associated factors that increased the risk of Mets (P<0.05). Meanwhile, high physical activity (OR = 0.321, 95% CI: 0.107–0.961) decreased the risk of MetS (P<0.05).
Conclusion: One-third of the hypertensive patients had MetS, thus highlighting the necessity of early screening and vigorous treatment of all hypertensive individuals to reduce the occurrence of cardiovascular events.
References
- Lindstrom M, DeCleene N, Dorsey H, Fuster V, Johnson CO, LeGrand KE, Mensah GA, Razo C, Stark B, Varieur Turco J, Roth GA. Global Burden of Cardiovascular Diseases and Risks Collaboration, 1990-2021. J Am Coll Cardiol. 2022 Dec 20;80(25):2372-2425. doi: 10.1016/j.jacc.2022.11.001. PMID: 36517116.
- World Health Organization, et al. Global report on hypertension: the race against a silent killer. 2023.
- Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet. 1997 May 24;349(9064):1498-504. doi: 10.1016/S0140-6736(96)07492-2. PMID: 9167458.
- Jordan Ministry of Health, Center for Strategic Studies, USAID, WHO. Jordan National Stepwise (STEPs) for Noncommunicable Diseases Risk Factors 2019 (2019) Jordan Ministry of Health. Retrieved from https://www.moh.gov.jo/ebv4.0/root_storage/en/eb_list_page/stepwise_survey_(steps)_2020_technical_report-english.pdf
- DeBoer MD, Filipp SL, Gurka MJ. Associations of a metabolic syndrome severity score with coronary heart disease and diabetes in fasting vs. non-fasting individuals. Nutr Metab Cardiovasc Dis. 2020 Jan 3;30(1):92-98. doi: 10.1016/j.numecd.2019.08.010. Epub 2019 Aug 24. PMID: 31662283; PMCID: PMC7393664.
- O'Neill S, O'Driscoll L. Metabolic syndrome: a closer look at the growing epidemic and its associated pathologies. Obes Rev. 2015 Jan;16(1):1-12. doi: 10.1111/obr.12229. Epub 2014 Nov 18. PMID: 25407540.
- Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC Jr; International Diabetes Federation Task Force on Epidemiology and Prevention; Hational Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; International Association for the Study of Obesity. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009 Oct 20;120(16):1640-5. doi: 10.1161/CIRCULATIONAHA.109.192644. Epub 2009 Oct 5. PMID: 19805654.
- Zhou MS, Wang A, Yu H. Link between insulin resistance and hypertension: What is the evidence from evolutionary biology? Diabetol Metab Syndr. 2014 Jan 31;6(1):12. doi: 10.1186/1758-5996-6-12. PMID: 24485020; PMCID: PMC3996172.
- Wilcox G. Insulin and insulin resistance. Clin Biochem Rev. 2005 May;26(2):19-39. PMID: 16278749; PMCID: PMC1204764.
- Osuji CU, Omejua EG. Prevalence and characteristics of the metabolic syndrome among newly diagnosed hypertensive patients. Indian J Endocrinol Metab. 2012 Mar;16 Suppl 1(Suppl1):S104-9. doi: 10.4103/2230-8210.94256. PMID: 22701827; PMCID: PMC3354939.
- Tachebele B, Abebe M, Addis Z, Mesfin N. Metabolic syndrome among hypertensive patients at University of Gondar Hospital, North West Ethiopia: a cross sectional study. BMC Cardiovasc Disord. 2014 Dec 6;14:177. doi: 10.1186/1471-2261-14-177. PMID: 25481843; PMCID: PMC4273452.
- Kant R, Khapre M. Profile of Metabolic Syndrome in Newly Detected Hypertensive Patients in India: An Hospital-Based Study. Int J Appl Basic Med Res. 2019 Jan-Mar;9(1):32-36. doi: 10.4103/ijabmr.IJABMR_108_18. PMID: 30820417; PMCID: PMC6385532.
- International Federation of Diabetes; 2006. Available from: http:// www.file:///C:/Users/acer/Downloads/IDF_Meta_def_final%20 (3).pdf. [Last accessed on 2023 Aug 10].
- World Health Organization. Obesity and Overweight. Available
- from: http://www.who.int/mediacentre/factsheets/fs311/en/. [Last accessed on 2023 Aug 12].
- World Health Organization. Global Physical Activity Questionnaire (GPAQ) Analysis Guide. World Health Organization http:// www.who.int/chp/steps/resources/GPAQ_Analysis_Guide.pdf (2020).
- Al Hadidi A. Prevalence of Obesity Among Adults in Jordan: National Survey iproc 2022; 8(1):e36398. doi: 10.2196/36398
- Obeidat AA, Ahmad MN, Haddad FH, Azzeh FS. Alarming high prevalence of metabolic syndrome among Jordanian adults. Pak J Med Sci. 2015 Nov-Dec;31(6):1377-82. doi: 10.12669/pjms.316.7714. PMID: 26870100; PMCID: PMC4744285.
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 2001 May 16;285(19):2486-97. doi: 10.1001/jama.285.19.2486. PMID: 11368702.
- Al-Shami I, Alkhalidy H, Alnaser K, Mukattash TL, Al Hourani H, Alzboun T, Orabi A, Liu D. Assessing metabolic syndrome prediction quality using seven anthropometric indices among Jordanian adults: a cross-sectional study. Sci Rep. 2022 Dec 6;12(1):21043. doi: 10.1038/s41598-022-25005-8. PMID: 36473903; PMCID: PMC9727133.
- Yasein N, Ahmad M, Matrook F, Nasir L, Froelicher ES. Metabolic syndrome in patients with hypertension attending a family practice clinic in Jordan. East Mediterr Health J. 2010 Apr;16(4):375-80. PMID: 20795419.
- Haverinen E, Paalanen L, Palmieri L, Padron-Monedero A, Noguer-Zambrano I, Sarmiento Suárez R, Tolonen H; Joint Action on Health Information (InfAct). Comparison of metabolic syndrome prevalence using four different definitions - a population-based study in Finland. Arch Public Health. 2021 Dec 23;79(1):231. doi: 10.1186/s13690-021-00749-3. PMID: 34949223; PMCID: PMC8697452.
- Akintunde AA, Ayodele OE, Akinwusi PO, Opadijo GO. Metabolic syndrome: comparison of occurrence using three definitions in hypertensive patients. Clin Med Res. 2011 Mar;9(1):26-31. doi: 10.3121/cmr.2010.902. Epub 2010 Aug 3. PMID: 20682756; PMCID: PMC3064758.
- Tadewos A, Egeno T, Amsalu A. Risk factors of metabolic syndrome among hypertensive patients at Hawassa University Comprehensive Specialized Hospital, Southern Ethiopia. BMC Cardiovasc Disord. 2017 Aug 8;17(1):218. doi: 10.1186/s12872-017-0648-5. PMID: 28789613; PMCID: PMC5549344.
- Naghipour M, Joukar F, Nikbakht HA, Hassanipour S, Asgharnezhad M, Arab-Zozani M, Mansour-Ghanaei F. High Prevalence of Metabolic Syndrome and Its Related Demographic Factors in North of Iran: Results from the PERSIAN Guilan Cohort Study. Int J Endocrinol. 2021 Mar 29;2021:8862456. doi: 10.1155/2021/8862456. PMID: 33859688; PMCID: PMC8024063.
- Boden G, Chen X, DeSantis RA, Kendrick Z. Effects of age and body fat on insulin resistance in healthy men. Diabetes Care. 1993 May;16(5):728-33. doi: 10.2337/diacare.16.5.728. PMID: 8495612.
- Ulasi II, Ijoma CK, Onodugo OD. A community-based study of hypertension and cardio-metabolic syndrome in semi-urban and rural communities in Nigeria. BMC Health Serv Res. 2010 Mar 19;10:71. doi: 10.1186/1472-6963-10-71. PMID: 20302648; PMCID: PMC2858142.
- Yanai H, Tomono Y, Ito K, Furutani N, Yoshida H, Tada N. The underlying mechanisms for development of hypertension in the metabolic syndrome. Nutr J. 2008 Apr 17;7:10. doi: 10.1186/1475-2891-7-10. PMID: 18416854; PMCID: PMC2335113.
- Lent-Schochet D, McLaughlin M, Ramakrishnan N, Jialal I. Exploratory metabolomics of metabolic syndrome: A status report. World J Diabetes. 2019 Jan 15;10(1):23-36. doi: 10.4239/wjd.v10.i1.23. PMID: 30697368; PMCID: PMC6347655.
- Lopez-Lopez JP, Cohen DD, Ney-Salazar D, Martinez D, Otero J, Gomez-Arbelaez D, Camacho PA, Sanchez-Vallejo G, Arcos E, Narvaez C, Garcia H, Perez M, Molina DI, Cure C, Sotomayor A, Rico Á, Hernandez-Triana E, Duran M, Cotes F, Leong DP, Rangarajan S, Yusuf S, Lopez-Jaramillo P. The prediction of Metabolic Syndrome alterations is improved by combining waist circumference and handgrip strength measurements compared to either alone. Cardiovasc Diabetol. 2021 Mar 22;20(1):68. doi: 10.1186/s12933-021-01256-z. PMID: 33752666; PMCID: PMC7986558.
- Xing Z, Peng Z, Wang X, Zhu Z, Pei J, Hu X, Chai X. Waist circumference is associated with major adverse cardiovascular events in male but not female patients with type-2 diabetes mellitus. Cardiovasc Diabetol. 2020 Mar 25;19(1):39. doi: 10.1186/s12933-020-01007-6. PMID: 32213183; PMCID: PMC7093979.
- Lanas F, Avezum A, Bautista LE, Diaz R, Luna M, Islam S, Yusuf S; INTERHEART Investigators in Latin America. Risk factors for acute myocardial infarction in Latin America: the INTERHEART Latin American study. Circulation. 2007 Mar 6;115(9):1067-74.
- doi: 10.1161/CIRCULATIONAHA.106.633552. PMID: 17339564.